It is a common misconception that implementing the Macy Catheter® at agencies involves incurring additional cost. In fact, use of this medication delivery technology reduces overall costs. The costs associated with utilization of the Macy Catheter are insignificant compared to the device’s clinical, quality, and cost-saving benefits.
When the oral route is compromised and ineffectively mitigates symptoms at end-of-life, alternate methods for medication administration like SL, IV, SubQ, and suppositories can ultimately be burdensome and costly. IV, SubQ, and suppository alternatives must be ordered, delivered, and set up, processes that can encumber patients, families, and clinicians with symptom control delays that may span hours or even days. Symptom control delays yield higher transfer rates to in-patient units, which can be a costly, arduous process.
When nurses encounter severe symptoms for which the sublingual route does not work, they often “chase” symptoms by titrating the dose and frequency of the sublingual medication before attempting a new route in an often futile attempt to control symptoms. This can take hours or even days. Symptoms not adequately controlled lead to increased triage calls and subsequent calls to prescribers and case managing nursing staff.
Incremental medication, delivery, and labor associated with these alternative methods of medication administration cost far more than the Macy Catheter. Since the catheter facilitates administration of medications already at the bedside, it allows for immediate control of symptoms without delays that consume nursing time. The catheter thus reduces patient/family burden and labor costs associated with “chasing symptoms.”
As operational costs continue to rise, patient acuity is trending higher; patients have more complex care needs and shorter lengths of stay, a duality that increases pressure on an already overburdened nursing staff.1 Technology that improves the ability to provide rapid symptom control while decreasing the cost and burden of care can help hospice agencies mitigate nursing staffing challenges.
Case Study: Hospice Buffalo
“A Cost and Quality Analysis of Utilizing a Rectal Catheter for Medication Administration in End-of-Life Symptom Management” describes how the use of the Macy Catheter at a large hospice in western New York has improved patient care and nursing efficiency while at the same time decreasing the cost of care.2
Hospice Buffalo provides routine hospice care in both private homes and long term care facilities and provides general inpatient care in a 22-bed hospice inpatient unit (HIU) in Erie County, NY. In 2016, the agency cared for approximately 4,134 hospice beneficiaries including 1,609 home care patients, 1,062 long term care/assisted living patients, 815 hospital patients, and 648 HIU patients.
Hospice Buffalo implemented the Macy Catheter program to pursue the goal of improving patient outcomes while simultaneously decreasing the burden and cost of care.
The agency cost of the Macy Catheters in 2016 was $0.15 per patient day ($25,415 in total cost for the Macy Catheter program divided by 168,054 total days of care). The cost of numerous parenteral medications has markedly increased over the last few years, and the pharmacy noted an alarming increase in parenteral medication costs in the HIU despite increased usage of the Macy Catheter in 2016.
In February 2017, Hospice Buffalo initiated Macy Catheter use guidelines in the HIU that included utilizing the Macy Catheter as the first line alternative when the oral route was not effective and asking families to bring in oral formulary medications from home when the patient came into the HIU. Their PBM costs resultantly declined by a dramatic 45%.
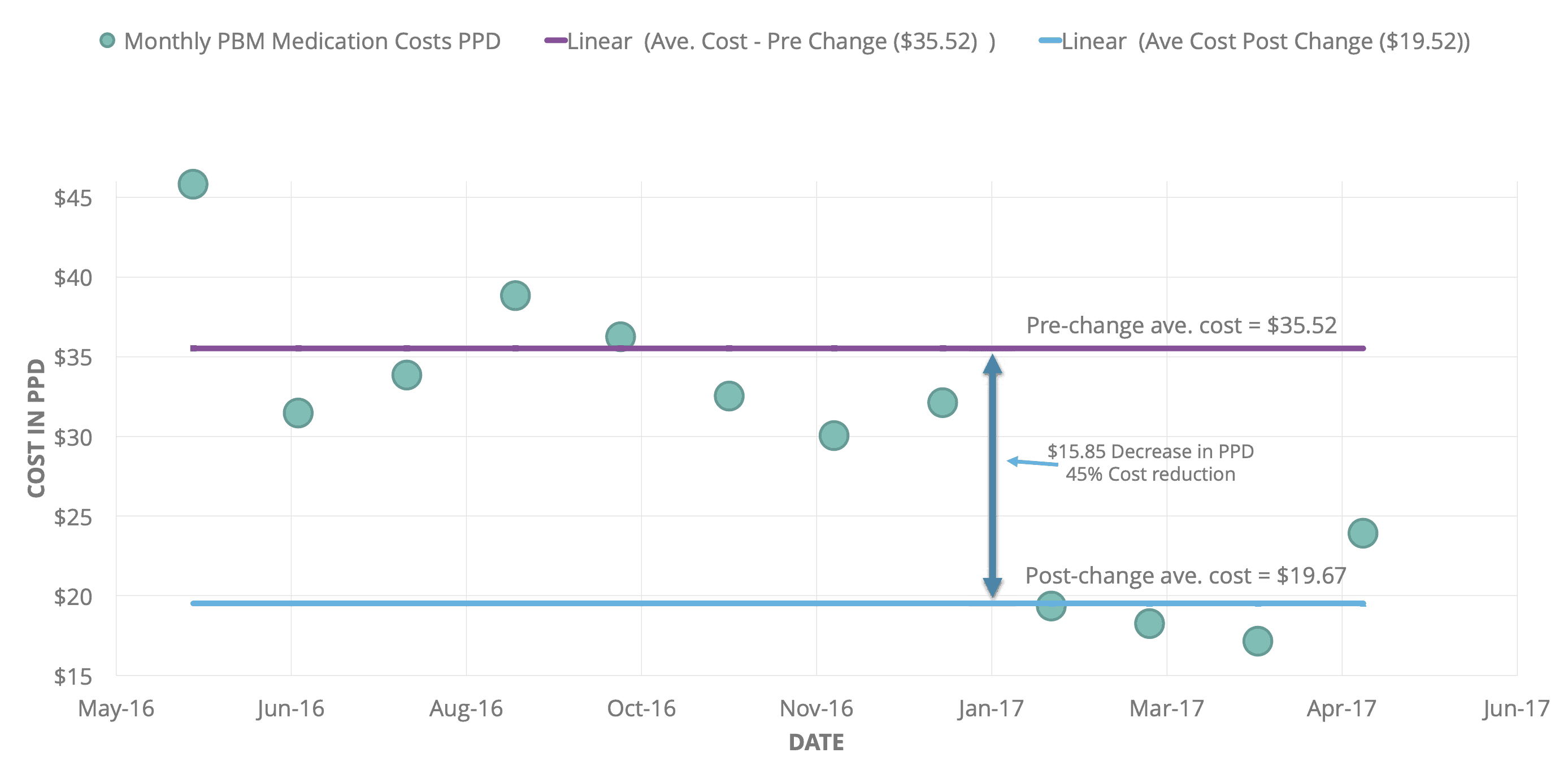
The annualized medication cost in the HIU prior to the policy change was $254,439. This cost dropped to $142,587 after the change. Therefore, there was an annualized gross savings of $111,852 in the HIU.
The ability to use medication in oral form already in the home is likely the biggest cost saving factor associated with the Macy Catheter in the home setting and in the HIU. This newfound ability also saves nursing time; medications in tablet form can be easily and quickly counted and disposed of. This process is much more tedious for parenteral medication.
At Hospice Buffalo, infusions are billed through an infusion pharmacy at a per diem rate that is separate from PBM costs incurred when using bolus-injected medication. Medication infusions and hydration incur a per diem infusion fee that costs an average of $40 per day, plus the cost of the medication and an additional infusion nurse visit charge if needed. The HIU at Hospice Buffalo slowly replaced medication and hydration infusions for medication and hydration via the Macy Catheter, resulting in a notable reduction in infusion expenditures. Between January 2016 and May 2017, PPD costs decreased by 16%, from an average of $1.85 to an average of $1.56.
The HIU manager and clinical staff at Hospice Buffalo reported that the Macy Catheter improved nursing efficiency due to a reduction in their usage of SubQ ports. They reported that SubQ ports take more nursing time to place and maintain than the Macy Catheter due to complexities associated with placement, labeling, site assessment, and occasional documentation of numerous ports per patient. Conversely, staff stated that Macy Catheter placement takes about five minutes. There is no associated maintenance unless the patient expels the catheter, in which case the catheter can be reinserted in just five minutes.
Hospice Buffalo found medication administered via the Macy Catheter to be comparatively less expensive and burdensome than the use of suppositories. There are numerous clinical downsides to using suppositories. These downsides include a lag prior to treatment, family and caregiver reluctance regarding usage, repositioning the patient and exposing private areas with each dose, discomfort with each insertion, and questionable or variable absorption in dehydrated patients. Suppositories require nurses to call the doctor and the pharmacy, check in on patient status, and assure patient comfort, so this medication administration method is more expensive, more burdensome, and less clinically beneficial than the Macy Catheter method.
Conclusion
The Macy Catheter can facilitate quick and effective symptom management while simultaneously decreasing costs, improving nursing efficiency, and decreasing the burden of care. The costs associated with utilization of the Macy Catheter are insignificant compared to the device’s clinical, quality, and cost-saving benefits. This effect is demonstrated by the cost reductions at Hospice Buffalo. More savings can be achieved with increased utilization.
[1] Hut, Nick, and Deborah Filipek. “Pressure Rising: Covid-19’s Ongoing Impacts on Healthcare Labor Trends.” Hfma, 5 Aug. 2021, www.hfma.org/topics/finance-and-business-strategy/article/pressure-rising-covid-19s-ongoing-impacts-on-healthcare-labor-trends.html.
[2] Natalie M. Latuga, Mary Gordon, Paula Farwell & Megan O. Farrell (2018) A Cost and Quality Analysis of Utilizing a Rectal Catheter for Medication Administration in End-of-Life Symptom Management, Journal of Pain & Palliative Care Pharmacotherapy, 32:2-3, 63-70, DOI: 10.1080/15360288.2018.1500509